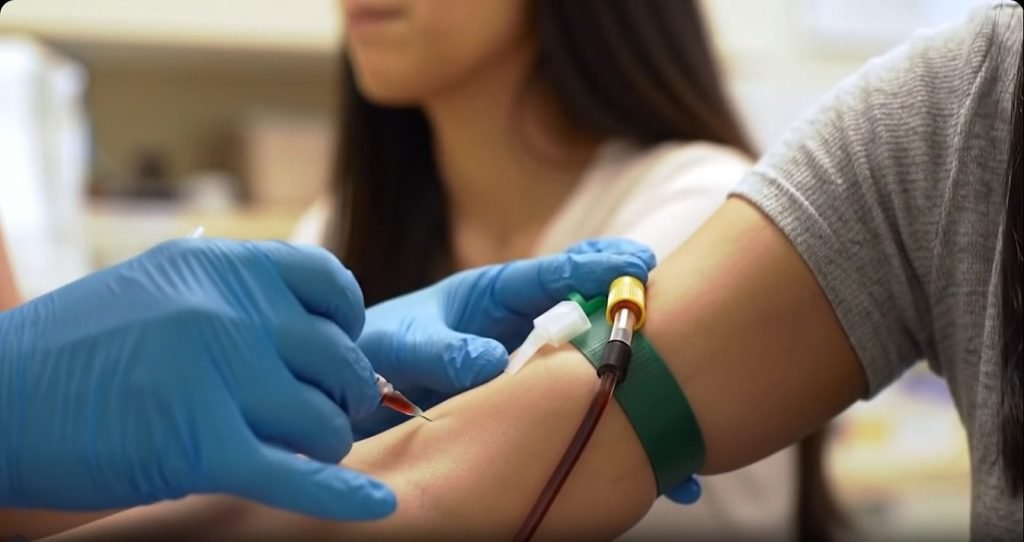
Sexually transmitted diseases (STDs), or sexually transmitted infections (STIs), often show no symptoms—making them easy to overlook. That’s why it’s essential to get tested for STD as soon as you see any related symptom. According to the World Health Organization (WHO), more than 1 million STIs are acquired globally every day, and many of these cases go undetected and untreated. https://www.who.int
“Ade, a 23-year-old undergrad, once walked into my clinic saying, ‘Doc, I feel fine, but I just came because my friend tested positive,’ I recall vividly. ” Her test came back positive too, and she had no symptoms at all.”
In Africa, cultural stigma and lack of access to reliable information mean many people avoid regular testing until symptoms become too serious to ignore. But taking charge of your sexual health isn’t just about avoiding illness—it’s about empowerment, prevention, and peace of mind.
Whether you’re sexually active in Nairobi, New York, or Lagos, here are 10 warning signs you should get tested for STD—and why waiting could put your health and that of your partner(s) at risk.
10 Warning Signs to Get Tested for STD
Had Unprotected Sex? Get Tested for STD Immediately
You don’t need multiple partners or a “wild lifestyle” to be at risk. Just one instance of unprotected sex—vaginal, anal, or oral—can expose you to infections like chlamydia, gonorrhea, HIV, or HPV.
“Condoms greatly reduce risk but are not 100% protective, especially against skin-to-skin infections like herpes or HPV,” says Dr. Aisha Balogun, a sexual health specialist in Lagos.
A 2022 study published in The Lancet emphasized that early testing after unprotected sex is the best strategy for limiting transmission and ensuring timely treatment. https://doi.org/
Strange Discharge? Don’t Ignore It, Test for STD
If you observe a change in your vaginal or penile discharge—such as an increased amount, foul smell, or strange color—it could be a sign of an infection like gonorrhea or trichomoniasis.
This symptom is often mistaken for a yeast infection or ignored entirely, especially among women.
“In many African societies, women are taught to normalize discomfort or assume discharge is part of menstruation or hygiene issues,” says Dr. Faith Mensah, a gynecologist based in Accra. “But that delay in seeking help often worsens outcomes.” Don’t delay; go test for STDs on time.
Genital Itching, Sores, or Bumps? Time to Check In
Itching may seem harmless, but persistent or painful itching in the genital area, along with visible sores or lumps, could signal herpes, syphilis, or HPV.
Herpes, in particular, can remain dormant and flare up unpredictably.
According to the Centers for Disease Control and Prevention (CDC), up to 87% of people with genital herpes don’t know they have it, making it one of the most underdiagnosed infections globally. https://www.cdc.gov/sti
Don’t self-medicate—get tested for STDs and treated early.
Started a New Relationship or Have Multiple Partners? Get a Test for STD
New relationships often come with passion—and risk. Even if you trust your partner, they may carry an infection unknowingly.
“You can’t tell someone’s STD status by looking at them. Testing should be a normal step before or soon after becoming sexually active with a new partner,” says Dr. Benson Nyaga, a sexual health educator in Nairobi.
Open conversations about testing may feel awkward, but they’re essential for healthy relationships.
Burning Urine? It Might Be an STI. Go Get Tested
Pain or burning during urination is commonly linked to urinary tract infections (UTIs), but it’s also a telltale sign of STIs like chlamydia or gonorrhea.
Left untreated, these infections can lead to serious complications such as pelvic inflammatory disease (PID) or infertility—especially in women.
According to the National Institutes of Health, up to 15% of women with untreated chlamydia develop PID, which can cause permanent damage to the reproductive system.
Painful Sex Isn’t Normal—Get a Checkup and Get Tested for STD
Painful intercourse, especially in women, may indicate an underlying STI like chlamydia, trichomoniasis, or even untreated pelvic inflammation.
It’s not something to power through.
Pain during sex is abnormal. In many African cultures, women endure in silence. We must shift that narrative,” says Dr. Thandiwe Ncube, an OB/GYN based in Johannesburg.
This symptom also occurs in men but is more common among female patients due to internal inflammation.
Irregular Periods or Pelvic Pain?
Heavy, irregular, or breakthrough bleeding—especially if accompanied by pelvic pain—could be related to an untreated infection.
This is particularly dangerous in countries where menstrual health is poorly monitored or misunderstood. STDs like gonorrhea and chlamydia can cause inflammation that disrupts the uterus.
If your cycle shifts unexpectedly, don’t ignore it—go test for STDs and talk to your doctor.
Your Partner Tested Positive—You Need To, Too
If your partner reveals they’ve tested positive for an STD or starts showing suspicious symptoms, go and test—even if you feel fine.
Many STDs are asymptomatic, and you could be a carrier without knowing it.
“Some people assume if they have no symptoms, they’re in the clear. But by the time symptoms show, damage may already be underway,” says Dr. Samuel Ochieng, public health researcher at Kenyatta University.
Mutual testing can help prevent reinfection and protect both partners’ long-term health.
History of STIs? Stay Ahead With Testing
If you’ve had an STD before, you’re at higher risk of getting another one, especially if you remain sexually active. Your immune system may also be more vulnerable to reinfection.
Routine testing—every 3 to 6 months—for sexually active individuals, especially those with past infections.
According to a 2023 WHO advisory, people with previous STIs are 2–3 times more likely to contract HIV due to mucosal damage and immune response factors. https://www.who.int/
Just Want Peace of Mind? That’s Reason Enough
This might be the most underrated reason for testing—but also the most empowering.
You don’t need to wait for symptoms to appear or partners to confess. Taking charge of your sexual health is about responsibility, self-respect, and confidence.
“Testing regularly is part of self-care,” says Dr. Aisha Balogun. “It’s just like getting a dental check-up or a Pap smear—except it protects you and others.”
Whether you’re celibate, sexually active, or somewhere in between, knowing your status helps you make informed decisions.
How Often to Test for STDs?
- Every 6 months if sexually active
- After any new sexual partner
- Immediately after unprotected sex
- If you experience any of the 10 signs above,
A Positive Result After Your Test for STD?
First: Breathe. Many STIs are treatable and manageable, especially if caught early.
- Treat it: Bacterial STIs like chlamydia, gonorrhea, and syphilis are curable with antibiotics.
- Manage Viral STIs: Herpes and HIV are manageable with proper treatment.
- Talk to Your Doctor: Don’t self-medicate. Get professional advice.

- Notify Your Partner(s): Prevent reinfection and protect others.
- Complete Treatment: Finish all medication—even if symptoms go away.
- Don’t Panic or Hide: You’re not alone. Many people live full, healthy lives after diagnosis. Read also: stress management
- Ensure Good Nutrition: Balanced nutrition helps maintain a strong immune system to combat infections. Read also: Boost immunity
How to Protect Yourself From STDs
- Use condoms consistently and correctly during vaginal, anal, and oral sex.
- Test regularly, especially if you’re sexually active or have multiple partners.
- Limit the number of sexual partners to reduce exposure risk.
- Engage in mutual monogamy with a partner who has tested negative.
- Vaccinate against preventable STDs like HPV and Hepatitis B.
- Avoid sharing sex toys, or sterilize them between uses.
- Practice good genital hygiene before and after sex.
- Avoid sex under the influence of drugs or alcohol, which can impair judgment.
- Communicate openly with partners about sexual history and STD testing.
- Seek prompt treatment if symptoms arise and complete any prescribed treatment.
- Encourage partner notification and treatment if you test positive.
- Educate yourself and others about STDs and how they spread
Final Thoughts: From Stigma to Strength
To test for STDs isn’t about fear—it’s about power. In Africa and around the world, STDs continue to carry shame and silence. But change starts with knowledge, openness, and action. Read also: Setting smart health goals
Whether you’re in Kampala, Cape Town, or London, remember: your body, your health, and your responsibility.
Test regularly for STDs. Share with a friend and normalize the conversation.
Be bold. Get a test. Stay safe. Share your journey in the comments.
This post is for educational purposes only; therefore, consult your doctor before making any health decision.
Kindly Subscribe, Like and Share this post.





Pingback: Home Remedies for Malaria in Nigeria: What Truly Works
Pingback: Chronic Urinary Tract and Prostate Disorders in Nigeria
Pingback: Common Women’s Health Disorders in Nigeria Explained
Pingback: HIV in Nigeria: Statistics, Symptoms, Treatment & Care