Chronic gastrointestinal disorders in Nigeria affect millions of people and significantly influence daily comfort, nutrition, productivity, and long-term health. Conditions such as stomach ulcers, hepatitis, chronic acid reflux, and functional bowel disorders are common, yet many people live with symptoms for years without proper diagnosis or treatment. Self-medication, delayed hospital visits, poor sanitation, and limited awareness often worsen outcomes.
This article explains ulcers, hepatitis, and chronic GI disorders in Nigeria, how these conditions develop, their common symptoms, health risks, diagnosis, treatment options, and practical steps for long-term care and prevention. The aim is to provide clear, trustworthy information that supports early recognition, safe care, and healthier digestive living.
Understanding Chronic Gastrointestinal (GI) Disorders
The gastrointestinal system includes the stomach, intestines, liver, pancreas, and related organs responsible for digestion, nutrient absorption, and waste removal. Chronic GI disorders are long-term conditions that affect one or more parts of this system and persist for months or years.
Unlike short-term digestive upsets that resolve quickly, chronic GI disorders tend to recur or persist, often requiring ongoing management. Symptoms may fluctuate, with periods of improvement followed by flare-ups. Without proper care, these conditions can lead to serious complications affecting nutrition, liver function, and overall wellbeing.
In Nigeria, chronic GI disorders are frequently underdiagnosed because symptoms are often normalized or treated with over-the-counter medications without proper evaluation.
Common Chronic GI Disorders in Nigeria
Several long-term digestive conditions contribute to the burden of chronic GI disorders across the country.
Stomach Ulcers (Peptic Ulcer Disease)
Stomach ulcers are open sores that develop in the lining of the stomach or the first part of the small intestine. They are among the most common chronic GI disorders in Nigeria.
The two leading causes of stomach ulcers are:
- Infection with Helicobacter pylori
- Prolonged or excessive use of painkillers such as non-steroidal anti-inflammatory drugs
Common symptoms include:
- Burning or gnawing stomach pain
- Pain that worsens when the stomach is empty
- Bloating or fullness
- Nausea
- Loss of appetite
Many people mistakenly attribute ulcer symptoms to stress or spicy food alone, delaying proper treatment. Untreated ulcers can lead to bleeding or perforation.
Hepatitis and Liver-Related GI Disorders
Hepatitis refers to inflammation of the liver and is a major contributor to chronic GI disorders in Nigeria. Viral hepatitis, especially hepatitis B and C, is common and often silent for many years.
Hepatitis affects digestion because the liver plays a key role in processing nutrients, detoxifying the blood, and producing bile for fat digestion. Chronic hepatitis may not cause symptoms until significant liver damage has occurred.
Common transmission routes in Nigeria include:
- Unprotected sexual contact
- Exposure to infected blood
- Unsafe injections
- Mother-to-child transmission
The World Health Organization notes that viral hepatitis often remains undiagnosed until advanced stages
Symptoms, when present, may include fatigue, abdominal discomfort, poor appetite, and yellowing of the eyes or skin.
Chronic Acid Reflux and GERD
Chronic acid reflux, also known as gastroesophageal reflux disease (GERD), occurs when stomach acid frequently flows back into the esophagus. This causes irritation and inflammation over time.
Common symptoms include:
- Persistent heartburn
- Sour taste in the mouth
- Chest discomfort
- Regurgitation of food
Dietary habits, obesity, smoking, stress, and late-night eating contribute to GERD. Untreated GERD can lead to esophageal damage and swallowing difficulties.
Irritable Bowel Syndrome and Functional GI Disorders
Irritable bowel syndrome (IBS) is a functional GI disorder characterized by abdominal pain, bloating, and changes in bowel habits without visible structural damage.
Symptoms may include:
- Abdominal cramps
- Diarrhea, constipation, or alternating patterns
- Bloating
- Gas
Stress, diet, and emotional factors play a significant role in IBS. While IBS does not cause permanent damage, it can significantly reduce quality of life.
Causes and Risk Factors of Chronic GI Disorders in Nigeria
Chronic GI disorders arise from a combination of infections, lifestyle factors, and healthcare practices.
Infections and Poor Sanitation
Infections play a major role in digestive diseases. H. pylori infection is widespread and closely linked to ulcer disease. Hepatitis viruses spread through unsafe blood exposure, poor infection control, and lack of vaccination coverage.
Unsafe drinking water, poor food hygiene, and inadequate sanitation increase the risk of repeated gastrointestinal infections that contribute to long-term digestive problems.
Medication Misuse and Self-Medication
Widespread self-medication contributes significantly to GI disorders in Nigeria. Overuse of painkillers irritates the stomach lining and increases ulcer risk. Unregulated herbal mixtures may damage the liver or interact with prescribed medications.
Delayed medical evaluation allows conditions to worsen before appropriate treatment begins.
Diet, Alcohol, and Lifestyle Factors

Dietary habits influence digestive health. Diets high in fatty, spicy, or heavily processed foods may worsen symptoms of reflux and ulcers. Excessive alcohol intake damages the stomach lining and liver, increasing the risk of ulcers and hepatitis complications.
Smoking further increases acid production and delays ulcer healing. Chronic stress affects gut motility and increases acid secretion, worsening GI symptoms.
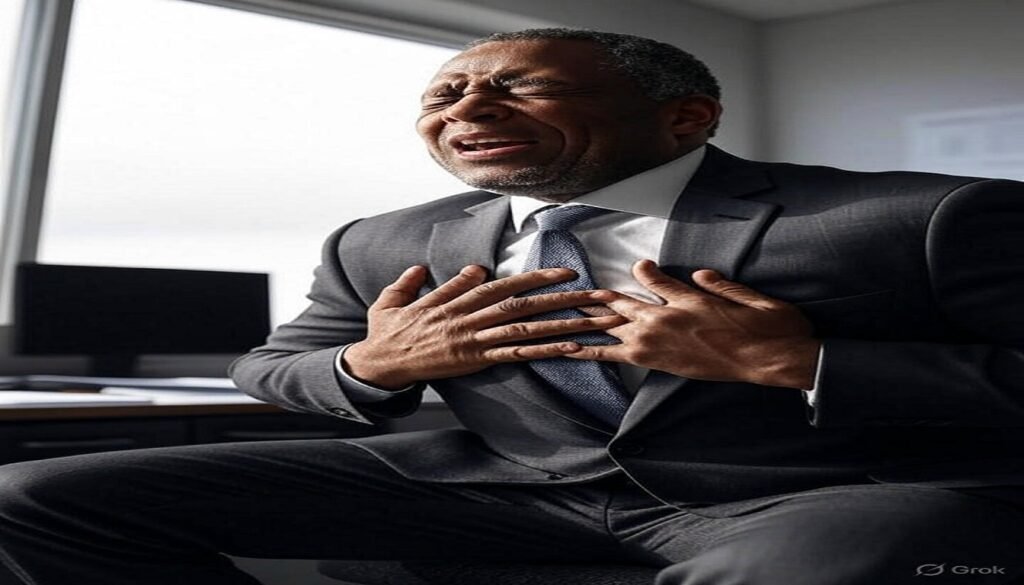
Common Symptoms and Warning Signs
Chronic GI disorders often present with persistent or recurring symptoms that should not be ignored.
Common warning signs include:
- Persistent or recurrent abdominal pain
- Heartburn or indigestion
- Nausea or vomiting
- Bloating or excessive gas
- Changes in bowel habits
- Unexplained weight loss
- Yellowing of the eyes or skin
- Dark urine or pale stools
Symptoms lasting several weeks or worsening over time require medical evaluation.
Health Risks and Complications
Untreated or poorly managed GI disorders can lead to serious complications.
Bleeding and Ulcer Complications
Stomach ulcers may bleed internally, causing black stools, vomiting blood, weakness, or dizziness. Severe ulcers can perforate the stomach or intestine, leading to life-threatening infection.
Liver Damage and Chronic Hepatitis Complications
Chronic hepatitis can progress silently to liver cirrhosis, liver failure, or liver cancer. Damage may only become apparent at advanced stages, emphasizing the importance of early detection and monitoring.
Impact on Nutrition and Quality of Life
Chronic digestive disorders interfere with nutrient absorption, leading to fatigue, weakness, anemia, and poor immune function. Persistent symptoms reduce appetite, disrupt sleep, and affect daily productivity.
How Chronic GI Disorders Are Diagnosed in Nigeria
Diagnosis begins with a detailed medical history and physical examination. Doctors may recommend tests based on symptoms and suspected conditions.
Common diagnostic approaches include:
- Blood tests to assess liver function and infection markers
- Stool tests for infections or bleeding
- Breath or stool tests for H. pylori
- Endoscopy to visualize the stomach and intestines
- Ultrasound or other imaging for liver and abdominal assessment
Early diagnosis improves treatment outcomes and prevents complications.
Living With Chronic GI Disorders in Nigeria
Living with a chronic GI disorder requires long-term management, but many people experience significant improvement with proper care.
Medical Treatment and Follow-Up Care
Treatment depends on the specific condition. Ulcers are treated with medications that reduce stomach acid and eradicate H. pylori. Hepatitis management may involve antiviral therapy and long-term monitoring. GERD treatment focuses on acid suppression and lifestyle changes.
Medication adherence and regular follow-up are essential. Avoiding self-medication and unverified remedies protects digestive and liver health.
The Federal Ministry of Health Nigeria emphasizes early diagnosis and appropriate treatment of digestive and liver diseases
Dietary Adjustments for GI Health

Dietary changes play a key role in symptom control. Helpful strategies include:
- Eating regular, balanced meals
- Reducing fatty, spicy, and acidic foods
- Limiting alcohol intake
- Avoiding late-night meals
- Practicing safe food handling and hygiene
Individual tolerance varies, so dietary adjustments should be personalized.
Lifestyle Changes and Symptom Control
Managing stress improves many GI symptoms, particularly in IBS and reflux disease. Adequate sleep, physical activity, and smoking cessation support digestive health and overall wellbeing.
Preventing Chronic GI Disorders in Nigeria

Prevention focuses on reducing exposure to known risk factors.
Effective strategies include:
- Safe drinking water and good sanitation
- Proper handwashing and food hygiene
- Hepatitis vaccination
- Responsible use of medications
- Limiting alcohol and avoiding smoking
- Early treatment of digestive symptoms
Public awareness and preventive care significantly reduce long-term disease burden.
When to See a Doctor for GI Symptoms
Medical care should be sought if symptoms persist, worsen, or include danger signs such as vomiting blood, black stools, severe abdominal pain, jaundice, or unexplained weight loss.
Early care improves outcomes and prevents life-threatening complications.
Common Myths About GI Disorders in Nigeria
Misinformation often delays proper treatment.
- Ulcers are caused only by stress.
Infections and medications play major roles. - Hepatitis is a spiritual illness.
Hepatitis is a medical condition caused by viruses or toxins. - Milk or herbs can permanently cure ulcers.
Proper medical treatment is required for healing and prevention.
Replacing myths with accurate information supports better health decisions.
Frequently Asked Questions
What are chronic GI disorders?
They are long-term conditions affecting digestion, the stomach, intestines, or liver.
Are stomach ulcers common in Nigeria?
Yes. H. pylori infection and medication misuse increase ulcer prevalence.
Can hepatitis be treated?
Many forms of hepatitis can be managed or treated, especially when diagnosed early.
How can people protect their digestive health?
Good hygiene, safe food practices, healthy diet, vaccination, and early medical care help protect digestive health.
When should GI symptoms be treated urgently?
Vomiting blood, black stools, jaundice, severe pain, or sudden weight loss require urgent medical attention.
Final Thoughts
Ulcers, hepatitis, and chronic GI disorders in Nigeria are common but manageable. Early recognition, proper diagnosis, safe treatment, and lifestyle care significantly improve outcomes and quality of life.
Digestive health plays a central role in overall wellbeing. Seeking timely medical care and avoiding harmful self-medication remain among the most important steps in protecting long-term GI health.
This article is for educational purposes only and does not replace professional medical advice.




Pingback: Vaccines in Nigeria: Protecting Our Children
Pingback: Top 20 Nigerian Remedies For Piles and Ulcers